The operating room is a special place where patients are treated. Statistically, the errors that top the list in the operating room are incorrect surgical sites, medication errors and foreign objects left in the incision. Therefore, perioperative patient safety has become a global concern. It is worthwhile for us to learn from the form of writing nursing record sheets in the operating rooms of American hospitals.
The nursing record sheets in the operating rooms of American hospitals are in the form of electronic version, and all the nursing records are done by entering into the computer. Therefore, all records are true, objective, timely and accurate.
Contents and types of records
01, Schedule of the surgical staff. Including the time of patient's arrival and departure, the time of the start and end of the operation, the number of operating table, the time of all the participants entering and leaving the operating room.
02, verification of the patient's identity always use "Y" and "N" to indicate the completion or not, including the confirmation of the patient's hospitalization number, fasting or not, infusion and whether there is a reaction to the infusion, unconsciousness, preoperative assessment and preoperative education completed. Form confirmations included: preoperative consent form, chest X-ray, electrocardiogram, laboratory tests, medical history, blood type, and type of blood product entered.
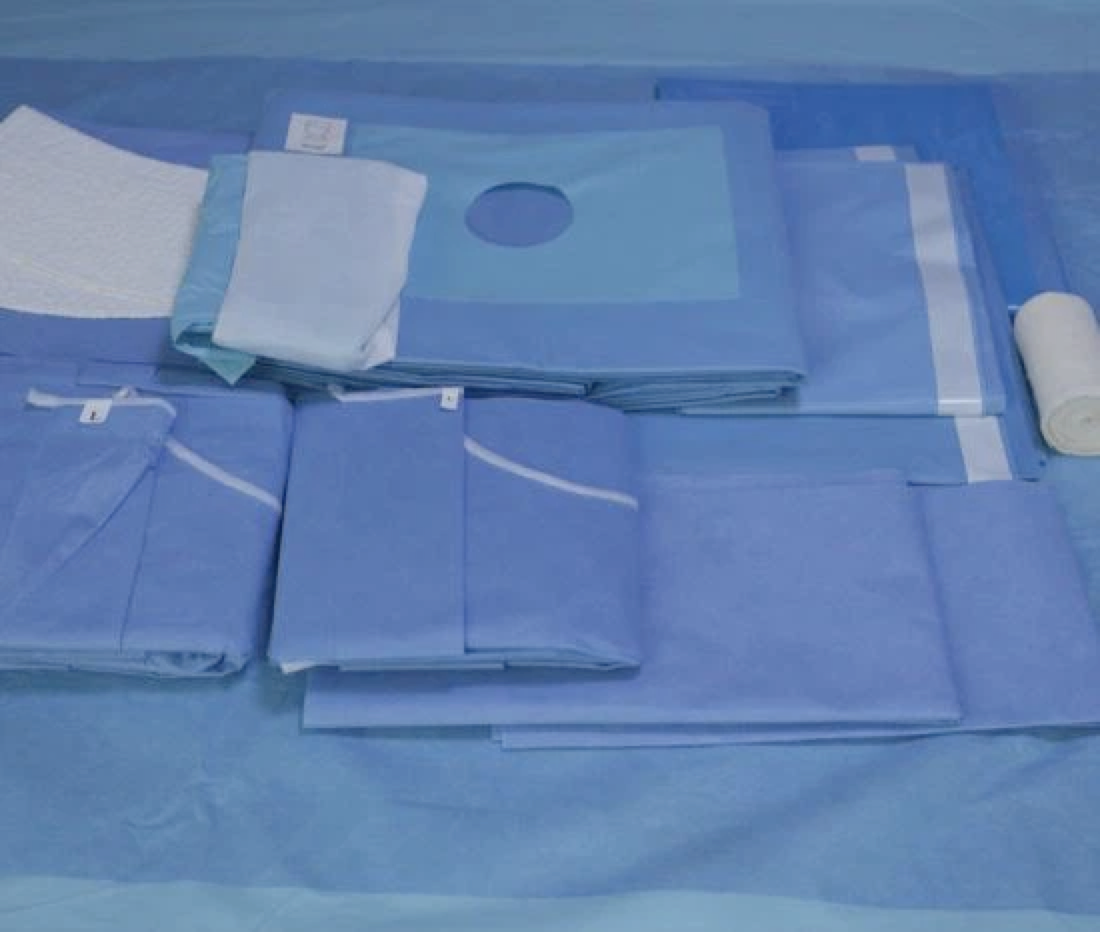
03. Preparation of the patient's skin and position. Including whether the skin is prepared, whether the skin is dry, with or without ulceration and oozing, the time of disinfection and sheet laying, the site of placement of the restraining belt, the patient's surgical position, the items used in the position, etc. will need to be described in detail.
04. Preparation of surgical instruments and application of tourniquet. If a tourniquet is required, the site of application of the tourniquet, whether it is padded or not, the pressure at the time of application, the start and end time should be indicated, and it should be signed by the responsible person.
05. inventory of surgical items. U.S. surgical instruments and utilization of the number of inventory is completed in a special work sheet, the work sheet is deposited in the patient's case, the contents of which include whether the preoperative hand-washing, itinerant nurses to jointly count twice and sign, before and after the closure of the body cavity to wash their hands, itinerant nurses to jointly check twice, to confirm that there is no error and then sign; if there is a hand-washing involved in the count in the middle of the itinerant nurses must be entered into the name to show that the responsibility for the separation of clear.
06, in and out of the volume, specimen and into the volume, including the amount of fluids, blood transfusion, intraoperative medication name, dose, route of administration, the use of antibiotics, name, time, dosage and mode of administration, and so on. Output includes the amount of bleeding, the type and size of urinary and gastric tubes, the amount of urine and the amount of gastric fluid drained and the amount of drainage. Specimens: first indicate the preoperative diagnosis and postoperative diagnosis, then indicate whether frozen specimens and specimen cultures are available, whether the specimens are properly placed, whether the wounds are graded, and the name, specification, number, and site of placement of the drains. Implants: when placing implants, then the name, specification, site, quantity are indicated, and the label of the time of implantation is all pasted on a special work sheet and deposited in the patient's case.
07. Postoperative situation. Whether the patient is conscious or not, the site of negative plate and tourniquet, whether the skin is intact or not, whether there is any damage to the skin other than the surgical area; if so, then the reason must be indicated. Whether the patient has returned to the ward and reconfirmation of the correct hospitalization number, etc.
08. Surgical handover and reconfirmation. The nurse in charge of the preoperative preparation room hands over and describes the preoperative patient with the traveling nurse. When the patient returns to the awakening room, the roving nurse and the nurse in the awakening room will then hand over and describe the patient's condition, and each will sign and confirm. Re-confirmation: that is, to remind again whether all the operations are correct, including whether the patient to verify the name, operation, site, position, implants, execution time, etc..
09, focusing on condition observation. At present, our existing nursing record sheets only have the checking of instruments and supplies, and there is no intraoperative nursing record. Therefore, itinerant nurses can easily neglect the changes in the patient's condition during the operation, such as infusion leakage, liquid go empty, limb pressure, urine bag burst full, etc., often observed only after the situation appears.
10, to ensure the safety of medication. Intraoperative medication, including the application of antibiotics, if there is no clear labeling in the nursing record sheet, when a dispute occurs, it will lead to the generation of insufficient evidence and responsibility for the phenomenon of unknown.
11, accurate handover. Before the start of surgery, before and after the closure of the body cavity need to check the instruments, dressings, if the circuit or hand washing nurses mid-shift inventory work, but did not sign to confirm, then when the problem occurs, the responsibility will be unclear phenomenon. In addition, when the roving nurses hand over to the nurses in the preparation room and the nurses in the awakening room, if the handover is not clear then it will lead to a handover error of the patient's condition, fluids, items and drains before and after the operation.