Surgical incision infections are divided into superficial incision tissue infections and deep incision tissue infections.
➤ Superficial incisional tissue infection
Infection involving only the skin or subcutaneous tissue of the incision that occurs within 30 d after surgery and meets one of the following conditions:
Inflammatory exudate from the superficial incision tissue;
Pathogens are cultured from fluid or tissue exuding from the superficial incision tissue;
Has signs or symptoms of infection, including localised redness, swelling, warmth, pain and tenderness.
➤ Deep incision tissue infection
Infections involving deep soft tissues (e.g., fascia, muscularis propria, cavities) that occur within 1 year of surgery in persons with implants and meet one of the following criteria:
Drainage or puncture of pus from a deep incision;
Isolation of causative organisms by culture from deep tissue punctures, secretions or tissues;
The deep tissue of the incision splits open on its own or becomes open to the outside. Also, the patient has signs or symptoms of infection, including localised fever, swelling and pain;
An abscess or other evidence of infection in the deep tissue of the incision is detected by clinical examination, re-operation exploration, pathology, bacteriology or imaging.
Principles of prevention
➤ Preoperative prophylaxis
① Evaluate the nutritional status and infection defence of the patient, comprehensive and detailed preoperative examination, preoperative patients with poor general condition (such as anaemia, hypoproteinemia) to improve the systemic condition, active treatment of the primary disease, and wait for the patient's physical condition to be strengthened before surgery;
② preoperative screening for coexisting foci of infection, treatment of potential foci of infection in the body: application of antibacterial drugs to patients suffering from tonsillitis, upper respiratory tract infections, urinary tract infections, tinea pedis infections, etc. to completely cure the foci of infection;
③ Assessment of the surgical area for scarring, history of surgery, skin psoriasis plaques, and vascular disease;
④ Preoperative skin preparation, showering is a better clinical practice and does not recommend chlorhexidine bathing or shaving;
⑤ Minimise the length of the patient's preoperative and postoperative stay to reduce the incidence of nosocomial infections.
➤ Operating theatre precautions
① Principle of minimising personnel flow in the operating room: strictly limit the number of surgical visitors and reduce personnel flow in the operating room;
② Normal operation of the laminar flow system to maintain a sterile environment;
③ Repeatedly rinse the incision, remove as much scar as possible when suturing, and pay attention to skin tension and alignment;
④ Use sutures containing triclosan antimicrobial agents when available, which have been shown to reduce the incidence of surgical site infections by about 30% in the literature and are recommended by the WHO, ACS and CDC guidelines to combat surgical site infections;
(5) Use of knotless sutures, when available, reduces both suturing and operative time, and results in uniform tension and good alignment of the incision;
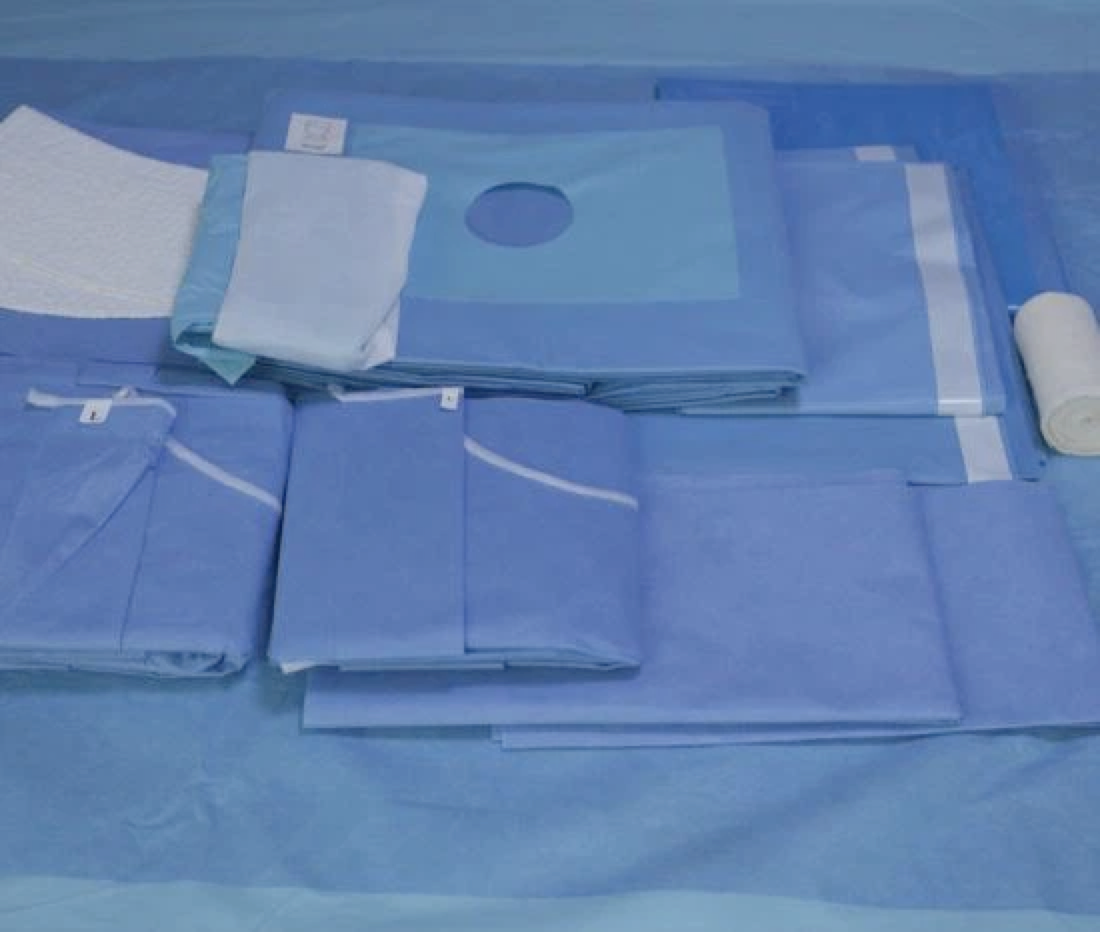
(vi) Use of bacteriostatic waterproof film absorbent pad dressings or visual waterproof foam dressings, isolation from the external environment, and showering, when available;
(vii) Use of a new type of skin adhesive with mesh when available, which can form an antibacterial barrier on the surface of the incision, preventing the entry of bacteria on the skin surface and from the outside world. No dressing is required after use;
(8) Drainage tubes can be used as appropriate according to the conditions; intraoperative bleeding tendency or trauma adjacent to the epidural patients can be routinely placed in the drainage tube, to keep the drainage tube clear to reduce the accumulation of blood (fluid) and reduce infection;
⑨ Prophylactic negative pressure wound therapy system can be applied when available.
➤ Postoperative preventive measures
① Observe the postoperative incision, reduce haematoma production, early incision of a small amount of oozing can be used to appropriate dressings;
② Improve postoperative nutrition and correct anaemia, enhance the body's ability to resist infection;
③ correct application of antimicrobial drugs to prevent infection, from skin incision to incision suture, to maintain sufficient antimicrobial drug concentration in the surgical field. The administration time is 30-120 min before the incision of the surgical site, and the antimicrobials are used after the operation as appropriate.
➤ Treatment recommendations
Infections in superficial parts of the incision can be cured by treatment with antimicrobial drugs and regular disinfection of the incision and dressing changes; deep infections are treated with drugs and debridement as appropriate. Retain the endophyte or endophyte removal and staged surgery.