Surgeons, in the eyes of internists, are cutters, only open the knife; in the eyes of internship students, clean, hands up, solve the patient's problem.
The first stage
The newborn calf is not afraid of tigers
Encountering intraoperative complications
In the fifth year of work, many of the first and second level surgeries can be master knife. One day, the emergency department newly admitted a chronic appendix:
1, middle-aged female patient, recurrent right lower abdominal pain for 2 years, reoccurrence of 1 day, previous consideration of appendicitis, are anti-inflammatory conservative treatment, this time intends to operate;
2, no previous history of hypertension, diabetes mellitus and other related medical history;
3, physical examination: abdomen flat, right lower abdomen pressure pain, rebound pain obvious;
4. Examination: leukocytes 12*10^9/L, ultrasound suggests inflammatory mass in the right lower abdomen, consider appendicitis;
5, Diagnosis: acute attack of chronic appendicitis.
Treatment: appendectomy.
Combined with several years of experience, the director was relieved to arrange: you can take your classmates to get it done.
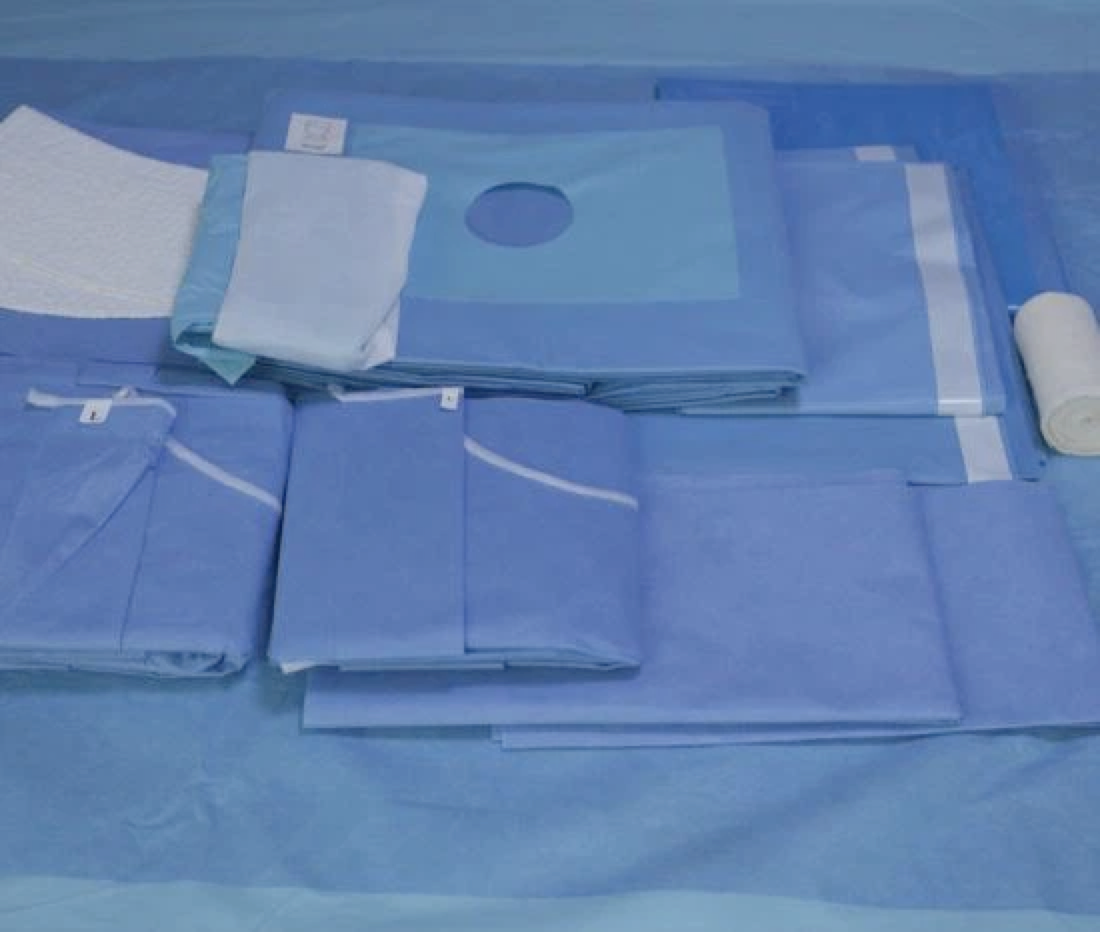
Anesthesia, disinfection, toweling, incision of the skin, fat layer, muscle layer, I sincerely hope that the appendix immediately jumped out, if you can not find the appendix for half an hour, it will be hairy in the heart, open appendectomy, the most difficult is not to cut the appendix, but to find the appendix.
For the peritoneum, three lifts and three releases, which was taught by the teacher during the internship, to prevent pinching the intra-abdominal tissue.
Second stage
Being able to act alone and maximize efforts
Facing patients with unsalvageable deaths
In 2015, the 8th year of work, 1 year back from Ruijin Hospital for further training in laparoscopy and breast surgery, confident and passionate about the future work.
A middle-aged male patient with steering wheel injury, pancreatic trauma combined with hemorrhagic shock, postoperative pancreatic fistula secondary to severe abdominal infection, emergency surgery. Early postoperative recovery was excellent, and he was already walking on the floor and starting to eat.
One night on the next night shift, the family called me and said the patient was not feeling well, the doctor on duty said it was fine and didn't deal with it, I called the director, who thought that the patient didn't have any abdominal pain, bloating, or fever, and the infection indicator on the blood draw wasn't high enough to worry about;
For the first time there was an argument with the director, and helplessly cried ......
The deterioration of the disease progressed very quickly, and communicated with the family that the condition was beyond my ability to recommend transferring to the hospital, and then transferred to the ICU of the higher hospital, and also failed to return.
At that time, I suddenly hated the general surgery department, there are things that I can not control even if I try very hard, in July I wanted to resign, I wanted to leave there, in August to submit a letter of resignation, in September to leave the hospital.
The hospital has not changed, the change is myself, resigned from the public hospital, what will happen in the future, I simply do not know, take one step at a time!
Stage 3
Have a strong heart
Learn from failure and continue to dive
Chose a private hospital, engaged in trauma repair, worked for 8 months, and realized that my favorite is still general surgery.
In June 2016, entered the general surgery department of Foshan Zen Medical Center, night shift independently did a lot of emergency critical and difficult patients surgery, recovery is very good;
In July 2023, faced with a 38-year-old patient with perianal perineal necrotizing fasciitis on the operating table, I knew that the mortality rate of this disease is as high as 22-40%.
As the most senior title doctor, I have intraoperative ambivalence: extensive incision and debridement, this is a diagnostic and treatment guidelines and expert consensus, if I do this, I have no bottom line in my heart, the patient died, and there are guidelines to do the endorsement;
If I use my own small incision + closed negative pressure drainage, can avoid extensive skin necrosis, and do not need to perform enterostomy, if the patient died, I may be legally responsible, may be revoked license to practice medicine, or even jail.
The patient was lucky, and so was I. He pulled through, and was discharged from the hospital in 56 days with no complications, avoiding surgery such as an enterostomy.